These Boobs Are All Me: Double Mastectomy and DIEP-Flap without Nipple
Updated May 28, 2024
Content created for the Bezzy community and sponsored by our partners. Learn More
Illustration by Brittany England
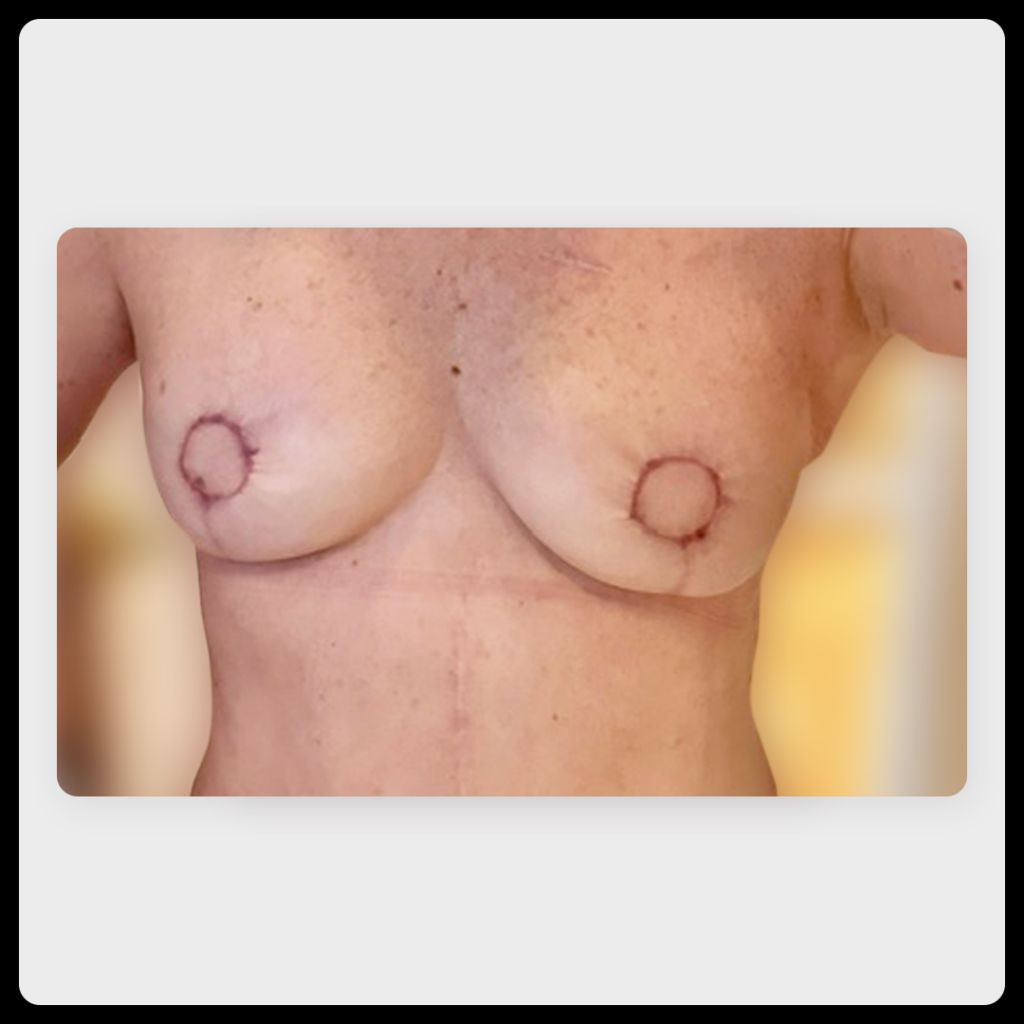
After battling breast and pancreatic cancer, I’m thrilled with my final result after DIEP-flap reconstruction. Next on the list is 3D nipple tattoos.
- Procedure: skin-sparing double mastectomy, reconstruction without nipple
- Reconstruction immediately post-mastectomy: yes
- Year of procedure: 2018
- Age: 55
- Ethnicity: white
This article contains graphic, intimate images of a postsurgery body. The photos have been generously shared by a breast cancer survivor so that others can benefit from uncensored visual information that may help them make important surgical decisions for themselves.
In 2010, my sister was diagnosed with stage I invasive ductal carcinoma and tested positive for the BRCA2 mutation. The rest of our family got tested, and I found out I was positive as well. I was about 44 at the time.
I had my ovaries removed at the age of 45 due to the high risk of ovarian cancer in BRCA2 carriers. I started breast surveillance with contrast-enhanced mammograms and MRIs from 2010 to 2022.
I was proactive, and I knew a preventive mastectomy was in my future. I wanted to do everything I could to detect cancer early, so we did routine screening every 6 months.
I always had the mastectomy in the back of my mind, but life gets in the way. There’s never really a good time to recover for 3 to 6 months.



Life speeds things up
Then COVID-19 hit, and my sister’s husband was lost to cancer in the midst of it. Then, my sister started having back pain. Even though all of her surveillance had come back negative, she was suddenly diagnosed with stage IV cancer.
I flew out to help, but she ended up passing away in December 2020, just a few days shy of her 60th birthday.
It was a really emotional time for me.
When I returned, I was exhausted. I was depressed. I felt like I was 10 weeks pregnant. I couldn’t get off the couch.
I had to reschedule a mammogram I’d pushed off to help my sister, and I found myself scared and wanting a full-body MRI. I was questioning how my sister could have suddenly succumbed to cancer when she had every medical option available to her.
Then I started having pain in the upper left quadrant of my gastrointestinal tract. It came on like a light switch. But in the midst of COVID-19, it took 2 weeks to see a doctor.
He ordered a computed tomography (CT) scan and an endoscopy to check on the pain and to help ease my anxiety. The endoscopy came back with nothing, but an MRI showed something in my breast.
It took 3 weeks to get a biopsy, and the wait was excruciating.
More like this:
- Hindsight Is 20/20: Double Mastectomy and DIEP Flap Reconstruction without Nipple
- Second Time’s the Charm: Double Mastectomy and Implant Reconstruction without Nipple
- Finally Happy: Implant Reconstruction with Nipple Tattoo
- Feeling Unbalanced: Double Mastectomy with DIEP Flap, Implants, and Nipple Reconstruction
Two diagnoses at once
It turned out it was ductal carcinoma in situ (DCIS) stage 0. I was grateful it was only stage 0, but I knew at that point that I needed a double mastectomy.
Although I’d known exactly what type of surgery and reconstruction I wanted for years, I hadn’t amassed a team of surgeons. It was really nerve-wracking because I felt like I had to get that thing out of me.
Then I heard about a procedure, new at the time, called a DIEP-flap surgery. I’d been planning to do a TRAM flap like a dear friend of mine, but this new option meant I could spare my abdominal muscles. I knew I didn’t want to have implants.
In order to do a DIEP flap, the doctors do what’s called a CT scan angiogram to make sure the blood vessels of the abdominal area can handle it. When my result came back, it showed something in my pancreas.
Pancreatic cancers can be hard to see, but another endoscopy found a 3 cm mass. The doctor said he was pretty sure it was malignant.
Everything came to a screeching halt.
They sat me down and said, “Don’t worry about the breast cancer. We’ve got to go after this 1000%.”
Pancreatic cancer doesn’t have a high survival rate, so I did the most aggressive chemotherapy I could. My doctor recommended a type that could target breast cancer, too.

Putting off surgery might’ve saved me
The irony is I’d been beating myself up for not having the preventive mastectomy, but delaying it actually saved my life. If I had done it earlier, we might not have found the pancreatic cancer in time.
Before the surgery to remove half of my pancreas, I went back for one more MRI of the breast. It showed that the DCIS was gone. The chemotherapy that was treating my pancreas also knocked out the breast cancer.
That was really, really good news, and I didn’t have to rush into the mastectomy anymore. Some of my medical team advised that I should wait to see if the pancreatic cancer came back.
After a while, I was sick of being on constant screening. Each time I was in the MRI tube, I thought, “Will this be the time they find something?”
I became robotic, having moments when I didn’t think I’d make it past tomorrow. It’s a weird feeling.
Planning my mastectomy
We weren’t sure if my body could withstand the type of tension the DIEP flap requires after chemotherapy, but I really wanted it. I also had a vertical scar on my abdomen from the pancreas removal that the surgeons would have to work with.
I did lots of research and started working with a plastic surgery nutritionist, exercising, and eating well. I was finally able to have a double mastectomy and DIEP flap surgery at age 55.
Some hospitals use nerve blocks, but mine used narcotics, and I didn’t respond well. I threw up, which is something you don’t want to do when you’ve just had abdominal surgery.
The first 2 weeks of recovery were the hardest. You’re not supposed to move your arms over your head. I used a reacher-grabber tool if I needed to reach something.
I had a nurse stay over in case I needed her, and I used a recliner for over 6 weeks so I didn’t have to use my abdominal muscles to sit up. That allowed me to watch TV in a comfortable position and then recline to rest.
I had six drains, and one of them for an entire month. For the first week, we also used a wound vac to help prevent the incisions from opening back up.
Getting used to my new look
My chest was bigger than I wanted, and I needed a belly button after pancreatic surgery.
I let my body heal for 6 months and tried getting used to my breasts, but they just weren’t the size I wanted. I went through a second phase of operations to reduce my breast size.
It may seem superficial to worry about your size or think about getting your abdomen contoured, but body dysmorphia can come with the process. I had those issues beforehand, and they didn’t go away.
Even so, I’m glad that I was able to do autologous tissue reconstruction. I had nerve grafting, so I have sensation in my breasts, and I’ll get 3D nipple tattoos when I’m done with further surgeries.
The bottom line: I look fantastic. I really do. Every day I marvel at the fact that if you meet me on the street, you won’t be able to tell. And that they’re mine. It’s my tissue.
What I want others to know
I didn’t know how scary survivorship was going to be.
During treatment, you go from appointment to appointment with a sense of purpose. It’s the waiting that’s the hardest part.
I’m grateful when I put my head on the pillow at the end of another day.
Being informed has helped decrease my stress. No one should go into this without their eyes open. There’s so much information and support available online and on Instagram.
Of course, everyone has their own journey and way of doing things. There’s no right or wrong way. Just do it with open eyes.
Bezzy BC and Young Survival Coalition are partnering to create What It Looks Like, a series showcasing photographs of different breast reconstruction choices on bodies of all shapes, sizes, and colors.
We’re spotlighting breast cancer survivors’ reconstruction decisions and stories so that other women facing mastectomy surgery can see and hear about many different real-life outcomes.
If you’re a survivor who’d like to share your reconstruction (or flat closure) images and story, we’d love to hear from you. Just have your photos ready and fill out this submission form.
Images and stories will be anonymously published on BezzyBC.com.
Originally written March 27, 2024
Medically reviewed on May 28, 2024


Like the story? React, bookmark, or share below:
Have thoughts or suggestions about this article? Email us at article-feedback@bezzy.com.